I hate burns, always have. They hurt and it is difficult to get relief when treating them. As a former Special Forces Medic (18D) who still occasionally teaches Tactical Combat Casualty Care (TCCC), I don’t know many medics/corpsmen or anyone else really who likes to treat burns. In combat, they were one of the most terrifying or dreaded injuries that one could face and I consider myself fortunate to have never really treated severe burns while down range. Therefore, my knowledge has pretty much been limited to what I was taught in the Q-course. Just sayin’, it’s been a minute since then so I do not remember much from our classes on long-term burn care. In fact, after a quick survey of other medics and corpsmen during my last TCCC class, none of them remembered much beyond the general wave-tops. Teaching according to the TCCC guidelines focuses primarily on the type, severity and percentage of the body burned with a treatment of dry sterile dressings, pain management and IV therapy. Generally speaking, burns no matter how severe, are something that you as a medic, want to pass along to someone else as quickly as possible. Long-term care is risky and requires more supplies than are generally available. There is no part of me that wanted to take care of a burn patient. In fact, I believe the case should be made that the dedicated folks who work in burn units could be canonized as saints. I do not have the words to express my gratitude toward them for their compassion and dedication. All of this is a preface for my lessons learned from managing the long-term care of Two, my second oldest son. I feel like I should tell you here, as some sort of expectation management, in the grand scope of burns, he was not burned that bad, only about 1% of his body. But, they were circumferential burns and we learned a lot! And he made a full recovery. This article is about what I learned while treating his injuries.
For those who know my son this whole story will not really be a surprise. Some hard lessons were learned that day in January, 2021. For some context, Two has a very large hole dug in our backyard. It lies next to the large woodpile he has spent the better part of the last two years splitting which is itself adjacent to our chicken coup and fire pit. This multipurpose hole is sometimes utilized as a fighting position, sometimes a hideout and most recently, the planned entrance to a large tunnel system that I think would have connected to the neighbor’s yard. That proposal was denied on application. The best way to describe the type of kid he is, is, he asked for and received an ax for Christmas when he was 6 and I was comfortable letting him use it. Almost six years later, he splits wood for fun and as a stress reliever! On the day of the incident, the wife was working and I was attempting to complete a long-neglected project (custom bunk beds and built-in shelves, closet and drawers) in his upstairs bedroom, I heard the soft whimper of pain emanating from the driveway below. I could hear water running and the strained effort to avoid trouble from a mistake that could get a then 11-year-old grounded, or worse, only allowed supervised backyard activity which typically includes, splitting wood, shooting BB guns and in this instance, attempting to prepare lunch on his single burner camp stove he just got for Christmas. Two was attempting to sauté some wild onions and carrots in olive oil that he did not ask permission to use. Truth be told, I would probably have said yes anyway. As for the food, I am not sure what direction he was going but the wife is a personal chef and we all look up to her in amazement at the food she creates!
As the small cries of pain increased, and the denials for help became less believable, I moved down the stairs to ensure nothing too serious had happened. Two was running cool water over an obviously burned hand and the pain was reaching a level where parental intervention was not only welcomed but sought out. We moved into the house where I could properly inspect the wound and I began inquiring about what and how this happened. All the while the pain was reaching almost unbearable levels. By the time he could properly explain that he had spilled boiling hot olive oil on his hand, the blisters began to form. Initially, I did not think the burn was that extensive and I remembered an incident from our Special Operations Combat Medic (SOCOM) training in Tampa, FL. In that case, someone had a whole pan of hot oil dumped over him and the doctors and nurses were struggling to manage the pain; morphine was not working and the oil was still burning. I remember the doc asking for a large tub of mayonnaise from the cafeteria. The mayonnaise would act as a solvent to the oil on the skin and provide pain relief…at least that is how I remembered it. So instead of running the burn under the cool water I spread the mayo on it…It did NOT work as I was expecting and provided little to no relief! I, being a bit stubborn, tried it three or four more times and we had to wash the mayonnaise off after about 1 minute or so each time. I do not know if it may have helped remove some of the oil from the skin but, overall, I am not convinced that it helped at all.
While I was trying to decide if a trip to the emergency room was warranted, my wife came home and we began discussing our options. It looked bad, but honestly, I did not think that bad. Eventually, we decided we should go to the ER based on the location of the burns – his fingers, and the fact they were basically circumferential, or all the way around. I absolutely do not regret our decision. For me, burns are and will always be something I want to pass off to someone else! The pictures below were taken in the Emergency Room and the ones following will generally chronicle the long-term care process. (Warning: If you are a bit squeamish proceed with caution.)

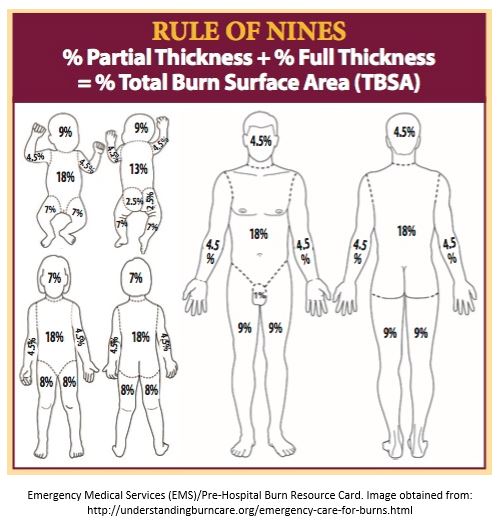
As you can see, the burns are almost circumferential and involve three digits, the little finger, ring finger and the finger or about 1% of the body surface area. I know that this post is really about long-term care but I would be remiss if I didn’t quickly cover acute care. From Understanding Burn Care (emphasis mine):
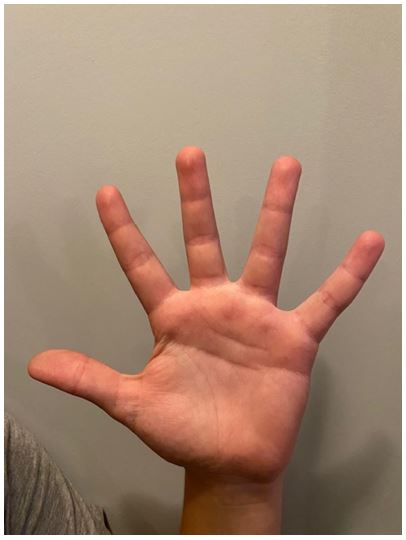
In general, minor burns are first-degree burns or second-degree burns that are smaller than the size of the patient’s hand. If the area burned is larger than this, or involves functional parts of the body such as feet, face, eye, ears and groin or is located over major joints, more in-depth medical attention is needed. Take the person to the nearest emergency room, family doctor or urgent care clinic to have the burn evaluated. Failure to do so may result in permanent disfigurement or loss of function.
Third degree burns are serious, regardless of size or area of the body that may be involved, and should be evaluated and treated by a qualified healthcare provider. All third-degree burns should be evaluated by a healthcare provider immediately. Burns that meet ABA burn center referral criteria are not minor burns and require specialized medical treatment.
They provide a nice chart also:
We were quickly admitted to the ER and and as soon as they established IV access they dosed him with morphine for pain relief. (I think they gave him 0.5mg or 1.5mg but I am not sure. Two is about 5’7” and weighs about 140lbs!) Pain management, other than cool running water was on board about 1 hour after the incident.
While we were waiting to be seen by the doctor, the nurse informed us that Wilmington, NC does not have a burn unit and the doctor would let me know what the treatment plan would be. I began to get a bit nervous, at this point a burn unit was not on my radar. As it turns out, Wilmington definitely does not have a burn unit, the closest one is in Chapel Hill, NC, and to have a bed saved for you it requires a ride in the ambulance. Two is a very brave young man. He rode in the ambulance by himself and I went home to gather my things for an overnight say. The wife would have to hold down the fort with the other littles. Prior to transfer, the nurse dressed the burns with bulky sterile dressings loosely wrapped around his fingers.
After about a two hour drive, we finally arrived at the University of North Carolina – Chapel Hill Hospital and settled in. The nurse immediately informed us that they would be conducting a cleaning and debridement that first night. The debridement included the removal of all the blisters. Occupational and Physical Therapists were also slated to stop by on the first night in the hospital.
For me, this is where the learning really began. Two was dosed with more morphine as they began to prepare for the initial debridement. The nurse gathered a wash basin, wash cloth, Johnson & Johnson baby soap and some minor surgery equipment that included tissue forceps and an iris scissors. To clean Two’s fingers, the nurse soaked the washcloth in the warm soapy water, folded it in 1/4s and wrapped the washcloth around each finger one at a time. She described the pressure as that of a firm but not hard handshake and pulled! All I can say is pain management is wonderful. I was relieved that Two barely flinched but the lack of reaction painted a different picture for the nurse. As she inspected further, the ‘skin’ below the blister barely blanched, didn’t have much feeling and barely bled. She was initially concerned the burn had exceeded the 2nd degree level and moved to a full thickness 3rd degree. By the time a doctor could come in and inspect the wound almost an hour later, the skin below the blisters ‘recovered’ a bit, began to blanch and even slightly bled. Two had severe second degree burns. Unfortunately, he did not let me take pictures during the initial debridement or the following morning.
Dressing Changes

Initially, the open areas on the skin were covered with Silvadene Cream (spread with a gloved hand) covered with sterile 2×2 gauze and loosely wrapped. Each finger was wrapped individually. This seemed sufficient until either physical therapy or occupational therapy, I cannot remember which, came in to test range of motion. They had Two go through several exercises and the bandages began to slip off. This required them having to be pushed back into place which was very painful. They redressed the wounds with an ‘anchor’ around the wrist holding them in place so the bandage would not slip.
The morning after the burn they wanted to do another dressing change and this time it would be my turn so I could demonstrate proficiency for my son’s release later that day if all went well. With the morphine out of his system this dressing change was considerably more painful. This time, the nurse put the Silvadene Cream directly on the 2x2s first and then wrapped it strait around the finger leaving it sort of bulky by the time the additional wraps were put in place. Once again, this worked but did not allow for enough range of motion in his exercises. Occupational therapy redressed the wound with less gauze, he completed his exercises and we were released.
It took me a little while to find the sweet spot for the right amount of Silvadene, too much squeezes out during his exercises, too little, the gauze sticks to the wound which makes the whole process much more painful. The following are pictures of my preparation and one of my better dressings.


How I did it.
I found the best way to dress the wound was to evenly spread the Silvadine on the unfolded 2×2 with a butter knife (the 2×2 was now a 2×4 rectangle). Think of spreading jelly on toast, not butter (too thin) or peanut butter (too thick). You do not want the antibiotic to squish out of the bandages. I would ensure that everything was prepped prior to starting the dressing change so that I could move as quickly as possible. Exposure to the air was generally not pleasant and I don’t think he really liked looking at it much.
I would then ‘candy wrap’ the finger with the 2×2 in a manner that is similar to the red stripe on a candy-cane. I would start at the base and wrap up. One bandage was the perfect size for each finger, his hands / fingers are about the average adult size. This allowed for maximum coverage with the minimum amount of bandage and provided for the maximum range of motion and proved to be the least painful.
To secure the 2×2 and keep the Silvadine from squeezing out, I would use a 2-inch gauze roll, start at the tip of the finger with only about half of the width of the bandage actually on the finger, wrap around one time then fold the access over holding it place with another wrap and then I would candy stripe down the finger at a maximum of double thickness. Once I reached the bottom of the finger, I would secure the bandage around the wrist going over the top of the hand. Most of the time. I had enough gauze in the roll to do one anchor wrap around the wrist, then move back up across the back of the hand and wrap one additional finger. This wasn’t always consistent and depended on how efficient I was wrapping each finger.
I would wrap the third finger similar to the first and secure the dressings in place with a stretchy tube shaped bandage. There were two sizes of the stretchy bandage, one for the fingers and one for the wrist.
Dressing changes were conducted daily in a manner similar to the burn unit. I would soak a washcloth in warm water that was mixed with Johnson & Johnson baby soap, fold the washcloth into 1/4s, wrap around the finger, apply firm but not hard pressure and pull…on each finger. He did not let me video it. The pictures below, chronicle the healing process up to our first trip back to the burn unit about 10 days post injury. I could not take a picture everyday because it was just too painful.




For me, the first really noticeable healing happened between 7 and 10 days post injury. During this period, his hand finally healed enough under the still attached but dead skin to allow for removal by the doctor at our follow up visit 10 days post injury with an iris surgical scissors. I removed some of the dead skin at the house but I don’t think Two trusted me enough to take most of it off.

Pain Management
Pain management is critical when dealing with long-term burn care and getting it right is not only important for the patient, but your sanity as well because, regardless of what drug combo you use, the dressing change process still hurts. In our case, the pain was primarily managed with Oxycodone plus Tylenol administered about 2 hours prior to the dressing change and again 4 hours later about an hour after the dressing change was complete and 600mg of Motrin 2-3 times a day for the first 10 days. After our trip to the doctor 10 days post injury we reduced the Oxycodone with Tylenol to just 2 hours prior to dressing change and Motrin as needed, typically once a day.




Our second trip to the burn unit was a success and Two was ready to move on from the daily dressing changes. From this point he was instructed to wear a compression glove to aid in the healing process and ensure that his hand did not swell during normal activities.


Physical / Occupational Therapy
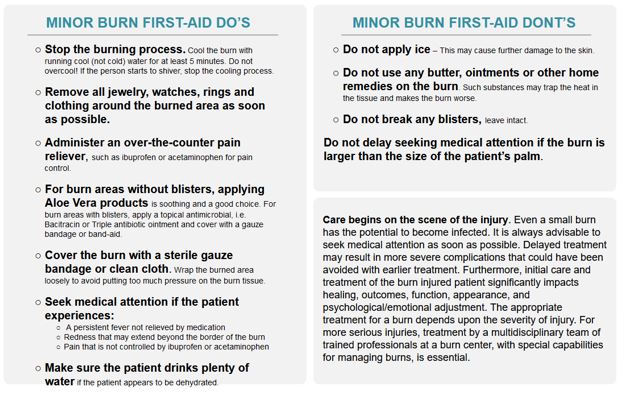
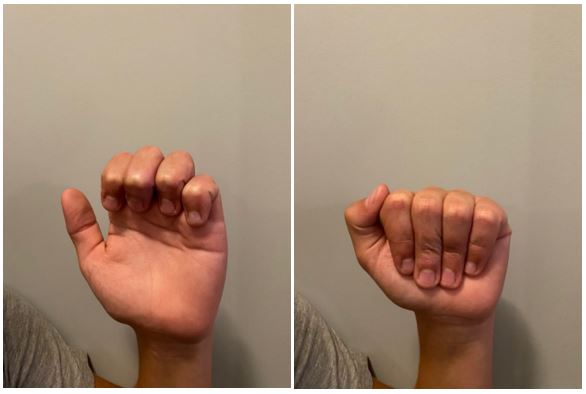
On the first day in the burn unit, not long after the initial debridement Physical and Occupational Therapy came in to inspect the injury and develop a plan for Two’s rehabilitation. Reducing their work to one paragraph does a disservice to their efforts but, basically, it boiled down to 4 exercises conducted in reps of 5, each held for ten-seconds, five times per day. Not only did they redress the wounds for maximum mobility, they demonstrated how to conduct the exercises and stressed the importance of doing so. Conducting this series of exercises was critical to maintain his full range of motion and healing from the incident. Every doctor and nurse that we encountered during this incident were amazing, but the Physical and Occupational Therapy folks really stood out in their knowledge and compassion! The pictures that follow demonstrate the exercises and the healing approximately 90 days post injury.

Ultimately, we were lucky and Two made a full recovery and we learned a lot in the process. I am glad that I had a medical background to lean on, however, I do not feel that my previous training was critical to our success. Anyone could do this. If there is one thing that I wanted you take from this, it would be to keep trying to improve your work, listen to your patient, and stick you your rehabilitation plan. The work that was required for what I initially thought was a relatively minor injury far exceeded my expectations. I am happy that I was able to be there for my son but I do not want to have to treat burns again!